Tag: team based care
Using art to heal
 Because Health is Life, our lifestyles are just as important to our health as going to the doctor or taking our medicines. In a paper published June 30, 2015 in the Annals of Internal Medicine, a study looking at survey data found that half the heart disease deaths in the US from 2009-2010 were caused by 5 factors all of which can be modified through healthy behavior: smoking, obesity, high cholesterol, diabetes and high blood pressure. But many of these behaviors are difficult to change and are influenced by our families, our culture and our community.
Because Health is Life, our lifestyles are just as important to our health as going to the doctor or taking our medicines. In a paper published June 30, 2015 in the Annals of Internal Medicine, a study looking at survey data found that half the heart disease deaths in the US from 2009-2010 were caused by 5 factors all of which can be modified through healthy behavior: smoking, obesity, high cholesterol, diabetes and high blood pressure. But many of these behaviors are difficult to change and are influenced by our families, our culture and our community.
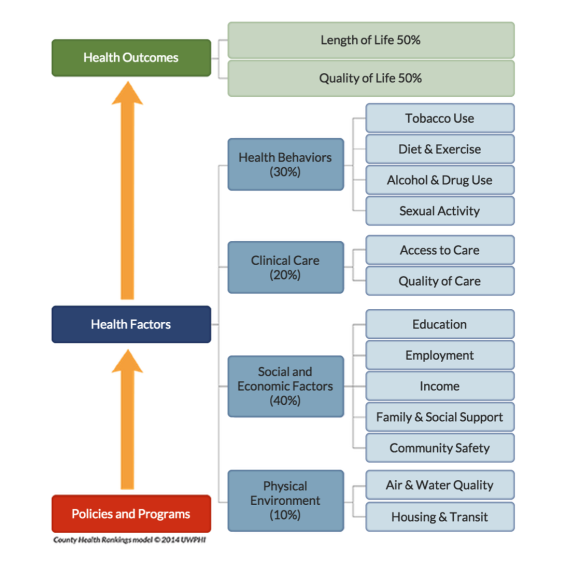
This picture shows that clinical care by doctors and hospitals accounts for only about 20% of health outcomes. The picture comes from a project called County Health Rankings developed by the University of Wisconsin Population Health Institute (and supported by the Robert Wood Johnson Foundation) that looks at health by county in the US. Addressing factors like cigarette smoking, income, education, employment, housing and clear air can help make communities healthier places to live.
We need to find ways to build healthier communities and the arts may be one way to accomplish this.
Patients and parents as partners – part II
 What if hospitals worked together to improve the care they deliver to patients with a particular disease (instead of competing with each other)? What if these hospitals considered patients and families their teachers and members of their teams? I’ve written before about the magic of the ImproveCareNow (ICN) network but even I am amazed at how quickly the interest in patients and parents as partners has grown within the network.
What if hospitals worked together to improve the care they deliver to patients with a particular disease (instead of competing with each other)? What if these hospitals considered patients and families their teachers and members of their teams? I’ve written before about the magic of the ImproveCareNow (ICN) network but even I am amazed at how quickly the interest in patients and parents as partners has grown within the network.
Parents as partners
 Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
I just returned from the ImproveCareNow Spring Learning Session where I saw all of this firsthand. ImproveCareNow (ICN) is a network of 64 (65 as of yesterday) care centers whose mission is to
Who makes the best medical student?
As I begin my 4th year interviewing prospective medical students, I am reminded of how challenging it is to figure out which applicants will possess all of the characteristics that I would want in my own doctor.
There is little question that we need to rethink the way we educate medical students to meet the needs of a changing healthcare system. Medicine is no longer a paternalistic practice where the doctor tells the patient what to do. Not only are patients becoming more empowered to participate in the own care, but they also have information at their fingertips about their own conditions and can access online discussion groups to talk with other patients about their shared experiences. The blog Wing of Zock looks at innovative ways to redesign medical education.
Redefining the care team
 When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
While it is certainly possible that these patients had an infectious disease that we don’t know about yet or that I had missed, many of them had significant stress in their lives – housing issues, trouble with their children or spouses, difficulites at work, etc. There is a lot of evidence that stress can lead to serious health issues including heart attacks.
The power of respect
Last week, I went to see my dermatologist for a full body check to make sure I don’t have melanoma. I showed up for my 3:00pm appointment a few minutes early and the receptionist said in a gruff voice, “You’re late. You had a 2:15 appointment. You can wait for the doctor to finish her office hours and be seen at the end of the day if you want”.
Hmmm….that was a little confusing since I had 3:00 in my calendar for many weeks – I made the appointment well in advance knowing that the dermatologist would need extra time for this type of appointment. So I told the receptionist that I thought there must be some mistake and asked if she could check again. By now she was really annoyed with me and said “No, you had a 2:15 appointment and it says right here that they tried to call you to confirm and your phone was out of service.” Now I was sure there was a misunderstanding since they had called to confirm my 3:00 appointment a few days earlier. So I asked her to please check that she had my name right. This time she said that I was correct (but did not offer an apology). She handed me some paperwork and said, in an accusing tone, that I was supposed to come every year and since I hadn’t been there in 3 years I had to fill out the medical history from scratch.
The whole patient
 During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.
During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.