Tag: research
Paying patients for their expertise
 Thanks to the work of organizations like the Society for Participatory Medicine and patient advocates like e-patient Dave, the voice of the patient is being heard. And I’ve written before about organizations like the ImproveCareNow network where patients and families are treated as equal partners in quality improvement efforts.
Thanks to the work of organizations like the Society for Participatory Medicine and patient advocates like e-patient Dave, the voice of the patient is being heard. And I’ve written before about organizations like the ImproveCareNow network where patients and families are treated as equal partners in quality improvement efforts.
I love that patients and families are being recognized for their expertise and that healthcare organizations are starting to involve patients as team members from the beginning of projects. I also love that organizations like PCORI (Patient Centered Outcomes Research Institute) are recognizing the importance of asking patients the research questions and outcomes that are most important to them.
So this is all really good, right? Yes, but…
The dark side of bacteria
Bacteria are our friends…but not all the time.
While I believe that we need to keep the bacteria in our bodies happy and that the improved cleanliness of modern life may be causing problems, there is also no question that bacteria are our enemies as well. You don’t have to look very far to see examples of how bacteria can cause serious illness or even death – meningococal meningitis, pneumococcal pneumonia, salmonella and tuberculosis to name a few. In most cases, antibiotics are required to treat these infections (or vaccines to prevent the infections).
Loving your bacteria
 When my kids were little, I used to joke that bacteria are our friends, so I didn’t worry much when their pacifiers fell on the ground. As an infectious diseases specialist I had also seen the harmful effects of using too many antibiotics – emergence of bad bacteria like MRSA (methicillin resistant Staphylococcus aureus) and development of diseases due to killing off of good bacteria (like Clostridium difficile colitis, a serious inflammation of the gut caused by antibiotics). So I also tried to avoid giving them antibiotics. New research suggests that bacteria may be more helpful than we ever knew.
When my kids were little, I used to joke that bacteria are our friends, so I didn’t worry much when their pacifiers fell on the ground. As an infectious diseases specialist I had also seen the harmful effects of using too many antibiotics – emergence of bad bacteria like MRSA (methicillin resistant Staphylococcus aureus) and development of diseases due to killing off of good bacteria (like Clostridium difficile colitis, a serious inflammation of the gut caused by antibiotics). So I also tried to avoid giving them antibiotics. New research suggests that bacteria may be more helpful than we ever knew.
Parents as partners
 Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
I just returned from the ImproveCareNow Spring Learning Session where I saw all of this firsthand. ImproveCareNow (ICN) is a network of 64 (65 as of yesterday) care centers whose mission is to
Redefining the care team
 When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
While it is certainly possible that these patients had an infectious disease that we don’t know about yet or that I had missed, many of them had significant stress in their lives – housing issues, trouble with their children or spouses, difficulites at work, etc. There is a lot of evidence that stress can lead to serious health issues including heart attacks.
Think before you eat
We may be eating in unhealthy ways without realizing it. Even healthy foods can lead to problems in certain people – for example dairy products in people who are allergic to them or wheat in people who have celiac disease. But even if food does not cause a bad reaction in us, there is research evidence that we are not in as much control of what we are eating as we think we are.
The first problem is that we often eat without thinking. Dr. Brian Wansink at Cornell University has done some fascinating experiments (which he writes about in his book, Mindless Eating) that look at why we eat more than we think. In one experiment he had people eat bowls of soup while he watched them using hidden cameras. For some people, more soup was piped into the bowl (without them knowing it) as they were eating – it was a bottomless bowl. These people ate more soup than those who had a regular bowl. Similarly, he has shown in experiments that people will eat less food if they use a smaller plate. In yet another experiment, he went to a movie theatre where a first-run movie was playing just after lunch on a Saturday. He prepared popcorn in advance and made sure it was really stale but still safe to eat. He offered each person who bought a ticket a free soft drink and a bucket of popcorn (some buckets were medium in size and some were large but all were too big to finish). People who got the large containers, ate more popcorn (even though it was stale). He surveyed people when they were leaving the theatre and most people who had the large buckets said that they would not be fooled into eating more popcorn by a larger bucket.
What’s the alternative?
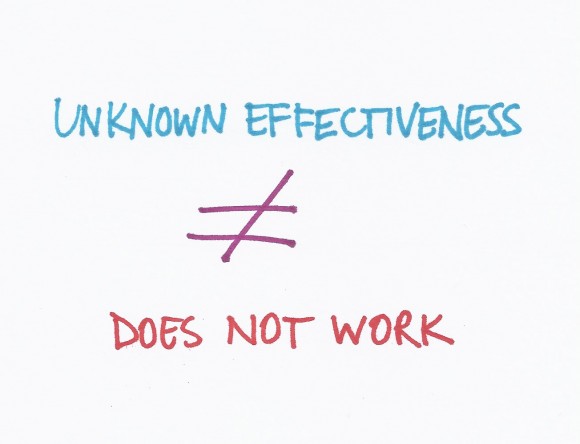
A recent blog post on The Health Care Blog entitled Choosing Alternative Medicine raises some really interesting issues. The author, James Salwitz, MD complains that patients are turning to complementary and alternative medicine (CAM) therapies when they could be cured by “conventional” therapy. I think the real problem is that people are being treated with therapies that have not been proven to work when there are other more effective treatments available. Patients need to be given enough information about the research evidence to make informed choices. After learning about the evidence, if they choose a therapy that has not been proven to work when there are more effective treatments available, I would consider that an informed decision.
Rather than saying some medicines are “alternative” and some are “traditional” we should look at all treatments for which there is evidence to treat a particular condition. If there is evidence that an herbal remedy or vitamin works even if it is not as good as the evidence for a drug, patients should be able to make the right choice for them based on the evidence. Doctors need to be open to thinking about CAM therapies as treatment options if there is evidence to support their use.
New types of evidence
It can be difficult to figure out how to use the results of research studies (randomized controlled trials or RCTs) to make a healthcare decision. There are many other problems with RCTs that may be less obvious.
First, to perform an RCT can take years – you need to get approval from the hospital where you are performing the study because you are doing research on humans. Then you need to get funding for the study so you may need to apply for some grants. After the study is completed, the results need to be analyzed; and then a paper needs to be written and submitted for publication to a journal. It could take years from the time the results are known until the time they are published.
Many commonly used treatments may not work
 A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
The way doctors determine if medical treatments work is to perform research studies called randomized controlled trials (RCTs). These are studies where half the patients get a treatment and half get a placebo (or inactive treatment like a sugar pill) but the patients and the researchers do not know who is getting what. After a period of time (could be years), the researchers look at the results and figure out which group did better.