Tag: doctor-patient communications
Does food cause inflammation?
I am fascinated by food – what makes us eat the food we eat and how it affects our health. I’m especially interested when there is evidence to support the ideas.
As the American diet has changed in the past few decades, we have been gaining weight. It is also true that we are seeing more diseases – especially those that have an inflammatory component. Inflammation is when the body responds to things that shouldn’t be there – like an infection or a chemical – and the body sends cells to the area to fight them off. This can lead to pain and swelling, among other things. Some diseases caused by inflammation have “itis” at the end – arthritis, colitis, bronchitis, etc.
Is it possible that the food we eat is causing some of these diseases that are due to inflammation?
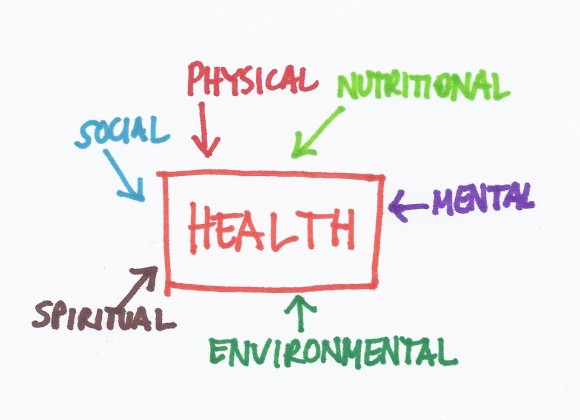
The whole patient
 During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.
During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.
Many commonly used treatments may not work
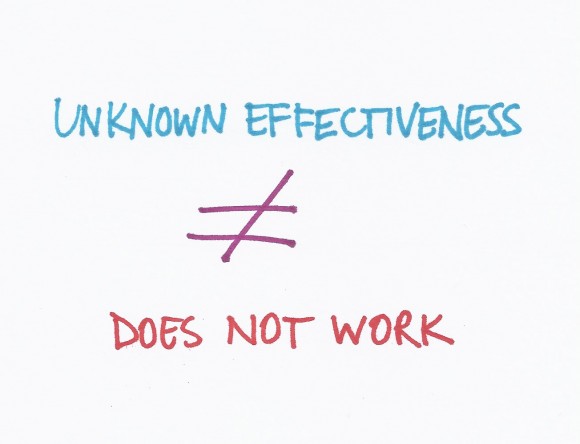 A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
The way doctors determine if medical treatments work is to perform research studies called randomized controlled trials (RCTs). These are studies where half the patients get a treatment and half get a placebo (or inactive treatment like a sugar pill) but the patients and the researchers do not know who is getting what. After a period of time (could be years), the researchers look at the results and figure out which group did better.