Tag: care redesign
Patient-collected data
 In April 2018, I participated in the 2018 Quantified Self (QS) Symposium on Cardiovascular Diseases held in San Diego. I was reminded of that session several weeks ago while attending the 2nd Annual Meeting of the Society for Participatory Medicine. In both conferences I was struck by the power of patients’ observations and measurements to manage their own diseases.
In April 2018, I participated in the 2018 Quantified Self (QS) Symposium on Cardiovascular Diseases held in San Diego. I was reminded of that session several weeks ago while attending the 2nd Annual Meeting of the Society for Participatory Medicine. In both conferences I was struck by the power of patients’ observations and measurements to manage their own diseases.
I first learned about the Quantified Self movement a few years ago while reading about Larry Smarr, an astrophysicist and computer scientist who started tracking his own exercise and weight but ultimately began expanding his self-tracking to include blood tests when he was told he had “pre-diabetes”. He ultimately diagnosed his own Crohn’s disease long before he had any symptoms based on analyzing his own blood and stool tests (including twice weekly stool microbiome analysis). He has since published a how-to guide in a biotechnology journal and participated in planning his own bowel resection for Crohn’s disease in 2016.
Using art to heal
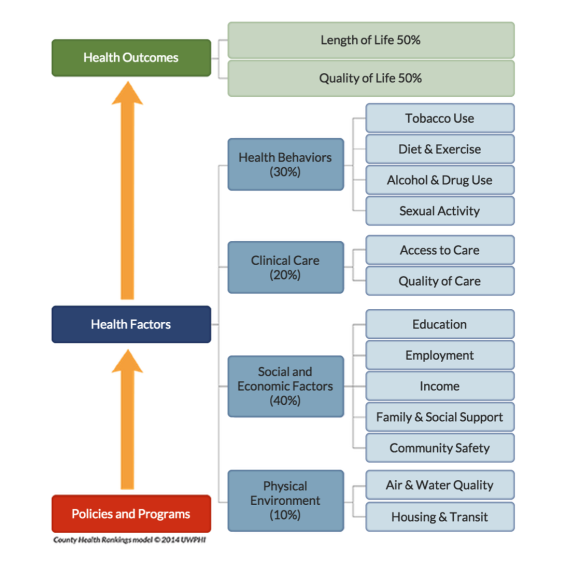 Because Health is Life, our lifestyles are just as important to our health as going to the doctor or taking our medicines. In a paper published June 30, 2015 in the Annals of Internal Medicine, a study looking at survey data found that half the heart disease deaths in the US from 2009-2010 were caused by 5 factors all of which can be modified through healthy behavior: smoking, obesity, high cholesterol, diabetes and high blood pressure. But many of these behaviors are difficult to change and are influenced by our families, our culture and our community.
Because Health is Life, our lifestyles are just as important to our health as going to the doctor or taking our medicines. In a paper published June 30, 2015 in the Annals of Internal Medicine, a study looking at survey data found that half the heart disease deaths in the US from 2009-2010 were caused by 5 factors all of which can be modified through healthy behavior: smoking, obesity, high cholesterol, diabetes and high blood pressure. But many of these behaviors are difficult to change and are influenced by our families, our culture and our community.
This picture shows that clinical care by doctors and hospitals accounts for only about 20% of health outcomes. The picture comes from a project called County Health Rankings developed by the University of Wisconsin Population Health Institute (and supported by the Robert Wood Johnson Foundation) that looks at health by county in the US. Addressing factors like cigarette smoking, income, education, employment, housing and clear air can help make communities healthier places to live.
We need to find ways to build healthier communities and the arts may be one way to accomplish this.
Health is life
When I was an infectious diseases specialist, most of the patients I saw were hospital inpatients but I also saw a few outpatients. They came to see me because of weeks or months of symptoms that their doctors couldn’t figure out and were often worried that they had a mysterious infection that was hard to diagnose. All of these patients had real symptoms – they were extremely tired, had headaches, muscle pains and sore throats. They generally arrived with stacks of medical records – numerous lab tests and notes from other doctors. I also noticed that many of them had serious “real life” problems – bad marriages, difficulties at work, housing problems, sick relatives and more. Perhaps they really did have an infection that I couldn’t find but I also began to wonder if their symptoms were caused by the stress.
My intuition was that many of these patients would benefit from speaking with a social worker, marriage counselor, psychologist, an expert in finding affordable housing or a financial planner. Unfortunately, these services were not part of our health care system. I suspected that many of my patients would get better if we were able to treat the whole patient, not just the symptoms.
Patients and parents as partners – part II
 What if hospitals worked together to improve the care they deliver to patients with a particular disease (instead of competing with each other)? What if these hospitals considered patients and families their teachers and members of their teams? I’ve written before about the magic of the ImproveCareNow (ICN) network but even I am amazed at how quickly the interest in patients and parents as partners has grown within the network.
What if hospitals worked together to improve the care they deliver to patients with a particular disease (instead of competing with each other)? What if these hospitals considered patients and families their teachers and members of their teams? I’ve written before about the magic of the ImproveCareNow (ICN) network but even I am amazed at how quickly the interest in patients and parents as partners has grown within the network.
Paying patients for their expertise
 Thanks to the work of organizations like the Society for Participatory Medicine and patient advocates like e-patient Dave, the voice of the patient is being heard. And I’ve written before about organizations like the ImproveCareNow network where patients and families are treated as equal partners in quality improvement efforts.
Thanks to the work of organizations like the Society for Participatory Medicine and patient advocates like e-patient Dave, the voice of the patient is being heard. And I’ve written before about organizations like the ImproveCareNow network where patients and families are treated as equal partners in quality improvement efforts.
I love that patients and families are being recognized for their expertise and that healthcare organizations are starting to involve patients as team members from the beginning of projects. I also love that organizations like PCORI (Patient Centered Outcomes Research Institute) are recognizing the importance of asking patients the research questions and outcomes that are most important to them.
So this is all really good, right? Yes, but…
Parents as partners
 Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
I just returned from the ImproveCareNow Spring Learning Session where I saw all of this firsthand. ImproveCareNow (ICN) is a network of 64 (65 as of yesterday) care centers whose mission is to
Are screening tests good for you?
If we had a serious disease, we’d like to learn about it before we even had symptoms (so we could get started on treatment). And most of us would like to know if we were at risk of developing a serious disease (so we could make changes to prevent the disease). Right?
Two recent articles in the NY Times point out the problems with screening tests.
Who makes the best medical student?
As I begin my 4th year interviewing prospective medical students, I am reminded of how challenging it is to figure out which applicants will possess all of the characteristics that I would want in my own doctor.
There is little question that we need to rethink the way we educate medical students to meet the needs of a changing healthcare system. Medicine is no longer a paternalistic practice where the doctor tells the patient what to do. Not only are patients becoming more empowered to participate in the own care, but they also have information at their fingertips about their own conditions and can access online discussion groups to talk with other patients about their shared experiences. The blog Wing of Zock looks at innovative ways to redesign medical education.
Redefining the care team
 When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
While it is certainly possible that these patients had an infectious disease that we don’t know about yet or that I had missed, many of them had significant stress in their lives – housing issues, trouble with their children or spouses, difficulites at work, etc. There is a lot of evidence that stress can lead to serious health issues including heart attacks.
