The gut and the brain
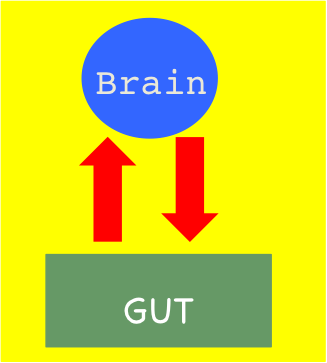 We don’t normally think about the gut and the brain being connected. And yet many of us have gotten a stomach ache, nausea or diarrhea from stress or a feeling of “butterflies” from excitement. Or we may experience pleasure from certain foods or feel a need to eat when under stress.
We don’t normally think about the gut and the brain being connected. And yet many of us have gotten a stomach ache, nausea or diarrhea from stress or a feeling of “butterflies” from excitement. Or we may experience pleasure from certain foods or feel a need to eat when under stress.
The vagus nerve travels between the brain and other organs in the body and can transmit messages in both directions. The brain can send messages to the gut through chemicals (called neurotransmitters). The gut has its own nervous system (called the enteric nervous system or ENS) that controls digestion. But scientists now think that the ENS can also produce neurotransmitters to send to the brain.
The big question is whether the gut can actually cause symptoms and diseases of the nervous system.
The power of placebos
 Lots of people talk about the placebo effect but what exactly is it?
Lots of people talk about the placebo effect but what exactly is it?
The most reliable clinical studies compare a treatment that is being tested with a fake treatment (called a placebo). Generally, half the people in the study get the treatment and half get the placebo and the then the two groups are compared. In the case of pills the placebo is often a sugar pill. Researchers can even test the effectiveness of a surgical procedure by comparing it with a sham or fake procedure. In these studies (called randomized controlled trials or RCTs), patients (and their healthcare teams) don’t know who is getting the pill or procedure being studied and who is getting the placebo. The reason for this is that patients sometimes get better when they are given a placebo because they believe they will get better (called the “placebo effect”) or because their disease got better on its own.
So can patients get better just by believing they will get better? And can doctors actually prescribe placebos to help people get better?
Research in real time
 This past week, I was reminded of the problem of fraud in medical research when the British courts ruled that the mother of a child with autism had lied about her child’s symptoms. The woman was a supporter of Dr. Andrew Wakefield, the British doctor who published studies connecting the Measles Mumps and Rubella – MMR – vaccine to autism based on “data” he made up.
This past week, I was reminded of the problem of fraud in medical research when the British courts ruled that the mother of a child with autism had lied about her child’s symptoms. The woman was a supporter of Dr. Andrew Wakefield, the British doctor who published studies connecting the Measles Mumps and Rubella – MMR – vaccine to autism based on “data” he made up.
Published medical studies, especially randomized controlled trials, remain the most reliable way for doctors to make treatment decisions. But, in addition to fraud, there are many other problems with medical research studies including the fact that they cost a lot of money to perform and take a long time to complete. An even bigger problem is that research studies have not been done for most of the questions that doctors and patients want answered. And even if there is a relevant published study, the people in the study may be very different from you.
FODMAPs
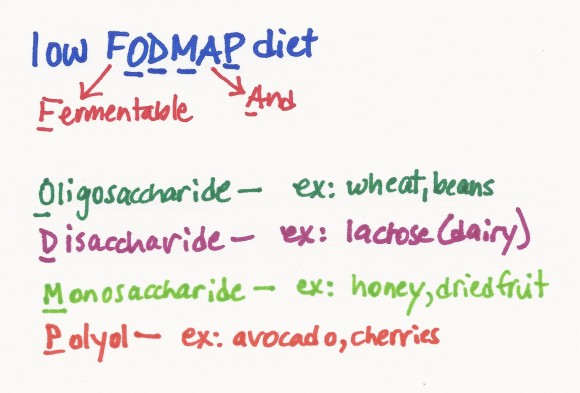 A few weeks ago, I was asked if I knew anything about the low FODMAP diet as a treatment for inflammatory bowel disease (IBD). I was sure this was yet another fad diet (or that the name was misspelled – seemed like FOD should be FOOD, right?) .
A few weeks ago, I was asked if I knew anything about the low FODMAP diet as a treatment for inflammatory bowel disease (IBD). I was sure this was yet another fad diet (or that the name was misspelled – seemed like FOD should be FOOD, right?) .
Imagine my surprise when I found detailed information about the diet and its use in treating irritable bowel syndrome (IBS) on the Stanford Health Care website. Irritable bowel syndrome is a chronic condition that causes abdominal pain, bloating, gas, diarrhea and other symptoms in the gut. It turns out that FODMAP is an acronym for Fermentable Oligosaccharide, Disaccharide, Monosaccharides and Polyol. All of these substances are found in certain foods and are types of carbohydrates. Researchers in Australia found that these carbohydrates are not well absorbed by the small intestine in people with IBS. As a result, the substances stay in the gut rather than being used by the body and they pull water into the gut. The FODMAPs can also be fermented by the bacteria in the gut which produces gas. All of this can lead to a bloating feeling, pain and other symptoms.
Patients and parents as partners – part II
 What if hospitals worked together to improve the care they deliver to patients with a particular disease (instead of competing with each other)? What if these hospitals considered patients and families their teachers and members of their teams? I’ve written before about the magic of the ImproveCareNow (ICN) network but even I am amazed at how quickly the interest in patients and parents as partners has grown within the network.
What if hospitals worked together to improve the care they deliver to patients with a particular disease (instead of competing with each other)? What if these hospitals considered patients and families their teachers and members of their teams? I’ve written before about the magic of the ImproveCareNow (ICN) network but even I am amazed at how quickly the interest in patients and parents as partners has grown within the network.
Paying patients for their expertise
 Thanks to the work of organizations like the Society for Participatory Medicine and patient advocates like e-patient Dave, the voice of the patient is being heard. And I’ve written before about organizations like the ImproveCareNow network where patients and families are treated as equal partners in quality improvement efforts.
Thanks to the work of organizations like the Society for Participatory Medicine and patient advocates like e-patient Dave, the voice of the patient is being heard. And I’ve written before about organizations like the ImproveCareNow network where patients and families are treated as equal partners in quality improvement efforts.
I love that patients and families are being recognized for their expertise and that healthcare organizations are starting to involve patients as team members from the beginning of projects. I also love that organizations like PCORI (Patient Centered Outcomes Research Institute) are recognizing the importance of asking patients the research questions and outcomes that are most important to them.
So this is all really good, right? Yes, but…
The dark side of bacteria
Bacteria are our friends…but not all the time.
While I believe that we need to keep the bacteria in our bodies happy and that the improved cleanliness of modern life may be causing problems, there is also no question that bacteria are our enemies as well. You don’t have to look very far to see examples of how bacteria can cause serious illness or even death – meningococal meningitis, pneumococcal pneumonia, salmonella and tuberculosis to name a few. In most cases, antibiotics are required to treat these infections (or vaccines to prevent the infections).
Loving your bacteria
 When my kids were little, I used to joke that bacteria are our friends, so I didn’t worry much when their pacifiers fell on the ground. As an infectious diseases specialist I had also seen the harmful effects of using too many antibiotics – emergence of bad bacteria like MRSA (methicillin resistant Staphylococcus aureus) and development of diseases due to killing off of good bacteria (like Clostridium difficile colitis, a serious inflammation of the gut caused by antibiotics). So I also tried to avoid giving them antibiotics. New research suggests that bacteria may be more helpful than we ever knew.
When my kids were little, I used to joke that bacteria are our friends, so I didn’t worry much when their pacifiers fell on the ground. As an infectious diseases specialist I had also seen the harmful effects of using too many antibiotics – emergence of bad bacteria like MRSA (methicillin resistant Staphylococcus aureus) and development of diseases due to killing off of good bacteria (like Clostridium difficile colitis, a serious inflammation of the gut caused by antibiotics). So I also tried to avoid giving them antibiotics. New research suggests that bacteria may be more helpful than we ever knew.
Parents as partners
 Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
I just returned from the ImproveCareNow Spring Learning Session where I saw all of this firsthand. ImproveCareNow (ICN) is a network of 64 (65 as of yesterday) care centers whose mission is to
