Category: Patients
What’s the alternative?
A recent blog post on The Health Care Blog entitled Choosing Alternative Medicine raises some really interesting issues. The author, James Salwitz, MD complains that patients are turning to complementary and alternative medicine (CAM) therapies when they could be cured by “conventional” therapy. I think the real problem is that people are being treated with therapies that have not been proven to work when there are other more effective treatments available. Patients need to be given enough information about the research evidence to make informed choices. After learning about the evidence, if they choose a therapy that has not been proven to work when there are more effective treatments available, I would consider that an informed decision.
Rather than saying some medicines are “alternative” and some are “traditional” we should look at all treatments for which there is evidence to treat a particular condition. If there is evidence that an herbal remedy or vitamin works even if it is not as good as the evidence for a drug, patients should be able to make the right choice for them based on the evidence. Doctors need to be open to thinking about CAM therapies as treatment options if there is evidence to support their use.
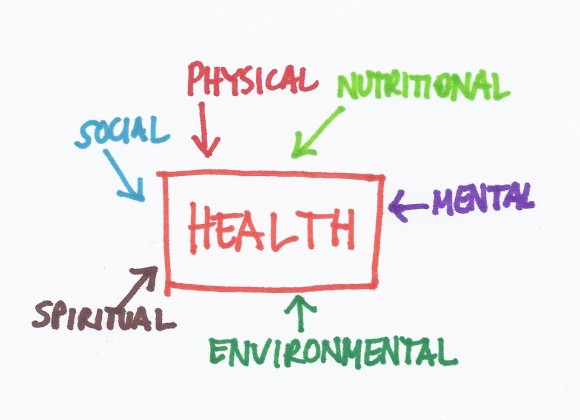
The whole patient
 During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.
During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.
Many commonly used treatments may not work
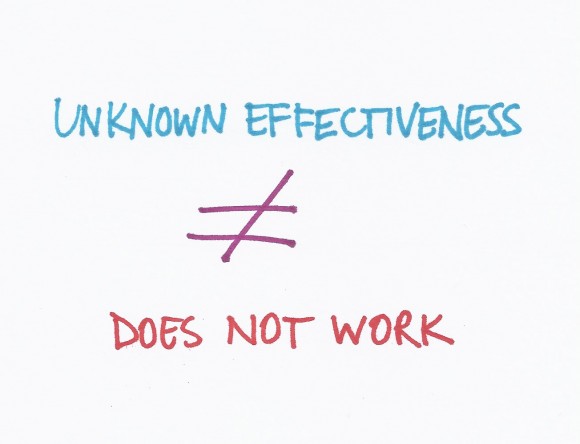 A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
The way doctors determine if medical treatments work is to perform research studies called randomized controlled trials (RCTs). These are studies where half the patients get a treatment and half get a placebo (or inactive treatment like a sugar pill) but the patients and the researchers do not know who is getting what. After a period of time (could be years), the researchers look at the results and figure out which group did better.
The Patient
 When I was a child, my parents were very friendly with their doctor who was an internist (someone who did medical training in internal medicine or general medicine for adults). Because he was a family friend, he agreed to start seeing me as a patient when I was about 12 years old. He was warm and friendly and took a long time to talk with me in his office before examining me. He did very few tests and almost never drew my blood.
When I was a child, my parents were very friendly with their doctor who was an internist (someone who did medical training in internal medicine or general medicine for adults). Because he was a family friend, he agreed to start seeing me as a patient when I was about 12 years old. He was warm and friendly and took a long time to talk with me in his office before examining me. He did very few tests and almost never drew my blood.
I remember those days fondly but they are long gone. My childhood doctor had far fewer tools at his fingertips and far less medical knowledge than we have today. Patients had very little access to the scant medical literature that was available. We put our trust in our doctors because they knew more than we did.