Category: Medical decisions
Research in real time
 This past week, I was reminded of the problem of fraud in medical research when the British courts ruled that the mother of a child with autism had lied about her child’s symptoms. The woman was a supporter of Dr. Andrew Wakefield, the British doctor who published studies connecting the Measles Mumps and Rubella – MMR – vaccine to autism based on “data” he made up.
This past week, I was reminded of the problem of fraud in medical research when the British courts ruled that the mother of a child with autism had lied about her child’s symptoms. The woman was a supporter of Dr. Andrew Wakefield, the British doctor who published studies connecting the Measles Mumps and Rubella – MMR – vaccine to autism based on “data” he made up.
Published medical studies, especially randomized controlled trials, remain the most reliable way for doctors to make treatment decisions. But, in addition to fraud, there are many other problems with medical research studies including the fact that they cost a lot of money to perform and take a long time to complete. An even bigger problem is that research studies have not been done for most of the questions that doctors and patients want answered. And even if there is a relevant published study, the people in the study may be very different from you.
Are screening tests good for you?
If we had a serious disease, we’d like to learn about it before we even had symptoms (so we could get started on treatment). And most of us would like to know if we were at risk of developing a serious disease (so we could make changes to prevent the disease). Right?
Two recent articles in the NY Times point out the problems with screening tests.
Giving thanks
 As Thanksgiving approaches, I am thinking a lot about the death of my father in early November 2011. I am thankful that my mother and I had the strength to bring him home to die with dignity, surrounded by his family. I feel blessed that my father lived a long, productive life and that he did not spend his last weeks or months in a hospital bed receiving treatment to prolong his life but not necessarily prolong the life he wanted to live.
As Thanksgiving approaches, I am thinking a lot about the death of my father in early November 2011. I am thankful that my mother and I had the strength to bring him home to die with dignity, surrounded by his family. I feel blessed that my father lived a long, productive life and that he did not spend his last weeks or months in a hospital bed receiving treatment to prolong his life but not necessarily prolong the life he wanted to live.
Death is not the enemy of life, it is a part of life. As Steve Jobs said in a commencement address at Stanford University in 2005:
No one wants to die. Even people who want to go to heaven don’t want to die to get there. And yet death is the destination we all share. No one has ever escaped it.
And yet, we often fight it, even when there is little hope of meaningful life.
The wisdom of patients
 Last week was the third anniversary of the death of my lifelong friend, Judy Feder. In 2001, Judy was diagnosed with Stage IV breast cancer at the age of 45.
Last week was the third anniversary of the death of my lifelong friend, Judy Feder. In 2001, Judy was diagnosed with Stage IV breast cancer at the age of 45.
I was involved in a health internet start-up at the time and knew about Gilles Frydman’s pioneering work in creating a collection of online patient communities called the Association of Cancer Online Resources (ACOR). Judy joined the group for patients with metastatic breast cancer. She embraced online communications (perhaps at least in part because she was a public relations professional) and participated in a second breast cancer online community called BC Mets as well. You can read about her 8-year breast cancer journey in this article in the Journal of Participatory Medicine, the journal of the Society for Participatory Medicine of which she was a founding member.
Does food cause inflammation?
I am fascinated by food – what makes us eat the food we eat and how it affects our health. I’m especially interested when there is evidence to support the ideas.
As the American diet has changed in the past few decades, we have been gaining weight. It is also true that we are seeing more diseases – especially those that have an inflammatory component. Inflammation is when the body responds to things that shouldn’t be there – like an infection or a chemical – and the body sends cells to the area to fight them off. This can lead to pain and swelling, among other things. Some diseases caused by inflammation have “itis” at the end – arthritis, colitis, bronchitis, etc.
Is it possible that the food we eat is causing some of these diseases that are due to inflammation?
What’s the alternative?
A recent blog post on The Health Care Blog entitled Choosing Alternative Medicine raises some really interesting issues. The author, James Salwitz, MD complains that patients are turning to complementary and alternative medicine (CAM) therapies when they could be cured by “conventional” therapy. I think the real problem is that people are being treated with therapies that have not been proven to work when there are other more effective treatments available. Patients need to be given enough information about the research evidence to make informed choices. After learning about the evidence, if they choose a therapy that has not been proven to work when there are more effective treatments available, I would consider that an informed decision.
Rather than saying some medicines are “alternative” and some are “traditional” we should look at all treatments for which there is evidence to treat a particular condition. If there is evidence that an herbal remedy or vitamin works even if it is not as good as the evidence for a drug, patients should be able to make the right choice for them based on the evidence. Doctors need to be open to thinking about CAM therapies as treatment options if there is evidence to support their use.
Many commonly used treatments may not work
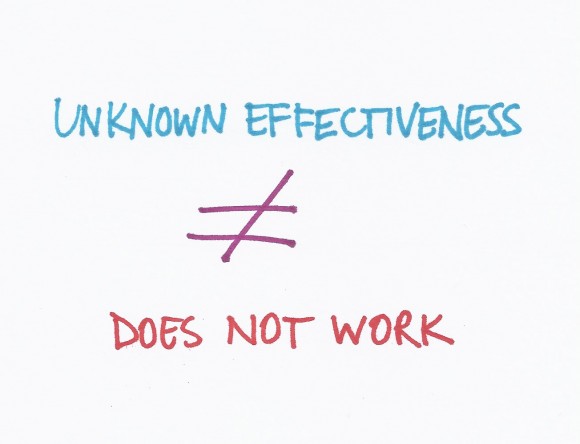 A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
A Washington Post WonkBlog piece entitled “Surprise! We don’t know if half our medical treatments work” got a lot of attention in social media circles. The title is a bit misleading but the concepts are really important. First, let me say that I worked at the BMJ for 8 years and was involved with the Clinical Evidence publication that is discussed in the blog so I may be a little biased!
The way doctors determine if medical treatments work is to perform research studies called randomized controlled trials (RCTs). These are studies where half the patients get a treatment and half get a placebo (or inactive treatment like a sugar pill) but the patients and the researchers do not know who is getting what. After a period of time (could be years), the researchers look at the results and figure out which group did better.