Category: Innovation
Parents as partners
 Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
Imagine a group of medical centers that share ideas and borrow from each other in order to improve the quality of the care they deliver. Imagine care teams where doctors, nurses, nutritionists, other health professionals and researchers work side by side with pediatric patients and their parents to figure out the best ways to deliver care. Imagine a healthcare conference where patients and parents are the teachers with doctors listening attentively and asking questions.
I just returned from the ImproveCareNow Spring Learning Session where I saw all of this firsthand. ImproveCareNow (ICN) is a network of 64 (65 as of yesterday) care centers whose mission is to
Who makes the best medical student?
As I begin my 4th year interviewing prospective medical students, I am reminded of how challenging it is to figure out which applicants will possess all of the characteristics that I would want in my own doctor.
There is little question that we need to rethink the way we educate medical students to meet the needs of a changing healthcare system. Medicine is no longer a paternalistic practice where the doctor tells the patient what to do. Not only are patients becoming more empowered to participate in the own care, but they also have information at their fingertips about their own conditions and can access online discussion groups to talk with other patients about their shared experiences. The blog Wing of Zock looks at innovative ways to redesign medical education.
Redefining the care team
 When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
When I was in clinical practice as an infectious diseases specialist, most of my patients were very sick and hospitalized but I saw a small number of outpatients as well. They were often people who had nonspecific complaints and were convinced that they had a chronic infection that their doctors were missing. They often arrived with numerous records – laboratory tests results, x-ray reports and consultation letters from other doctors.
While it is certainly possible that these patients had an infectious disease that we don’t know about yet or that I had missed, many of them had significant stress in their lives – housing issues, trouble with their children or spouses, difficulites at work, etc. There is a lot of evidence that stress can lead to serious health issues including heart attacks.
The wisdom of patients
 Last week was the third anniversary of the death of my lifelong friend, Judy Feder. In 2001, Judy was diagnosed with Stage IV breast cancer at the age of 45.
Last week was the third anniversary of the death of my lifelong friend, Judy Feder. In 2001, Judy was diagnosed with Stage IV breast cancer at the age of 45.
I was involved in a health internet start-up at the time and knew about Gilles Frydman’s pioneering work in creating a collection of online patient communities called the Association of Cancer Online Resources (ACOR). Judy joined the group for patients with metastatic breast cancer. She embraced online communications (perhaps at least in part because she was a public relations professional) and participated in a second breast cancer online community called BC Mets as well. You can read about her 8-year breast cancer journey in this article in the Journal of Participatory Medicine, the journal of the Society for Participatory Medicine of which she was a founding member.
More on technology (and communication)
There is no question that technology can improve the quality of healthcare but it can’t replace the need for good communication.
Dr. Peter Pronovost, a leader in patient safety at Johns Hopkins, wrote a blog post today about how technology can help doctors make the right diagnosis. He cites alarming statistics about how the wrong diagnosis may cause as many as 80,000 deaths each year in the US. He discusses the exciting news that a portable bedside device that is able to measure eye movements, may prove to be useful in emergency rooms to figure out which patients who complain of dizziness are likely to be having a stroke. This development could save lives and also save time and money.
However, in many of the cases of misdiagnosis, the problem is that doctors don’t listen carefully to what patients and their families are saying. They forget that patients are the experts about their own symptoms. Doctors have a tendency to get locked into thinking about a particular diagnosis and may not listen to what patients (and their families) are telling them.
Think before you eat
We may be eating in unhealthy ways without realizing it. Even healthy foods can lead to problems in certain people – for example dairy products in people who are allergic to them or wheat in people who have celiac disease. But even if food does not cause a bad reaction in us, there is research evidence that we are not in as much control of what we are eating as we think we are.
The first problem is that we often eat without thinking. Dr. Brian Wansink at Cornell University has done some fascinating experiments (which he writes about in his book, Mindless Eating) that look at why we eat more than we think. In one experiment he had people eat bowls of soup while he watched them using hidden cameras. For some people, more soup was piped into the bowl (without them knowing it) as they were eating – it was a bottomless bowl. These people ate more soup than those who had a regular bowl. Similarly, he has shown in experiments that people will eat less food if they use a smaller plate. In yet another experiment, he went to a movie theatre where a first-run movie was playing just after lunch on a Saturday. He prepared popcorn in advance and made sure it was really stale but still safe to eat. He offered each person who bought a ticket a free soft drink and a bucket of popcorn (some buckets were medium in size and some were large but all were too big to finish). People who got the large containers, ate more popcorn (even though it was stale). He surveyed people when they were leaving the theatre and most people who had the large buckets said that they would not be fooled into eating more popcorn by a larger bucket.
Does food cause inflammation?
I am fascinated by food – what makes us eat the food we eat and how it affects our health. I’m especially interested when there is evidence to support the ideas.
As the American diet has changed in the past few decades, we have been gaining weight. It is also true that we are seeing more diseases – especially those that have an inflammatory component. Inflammation is when the body responds to things that shouldn’t be there – like an infection or a chemical – and the body sends cells to the area to fight them off. This can lead to pain and swelling, among other things. Some diseases caused by inflammation have “itis” at the end – arthritis, colitis, bronchitis, etc.
Is it possible that the food we eat is causing some of these diseases that are due to inflammation?
The whole patient
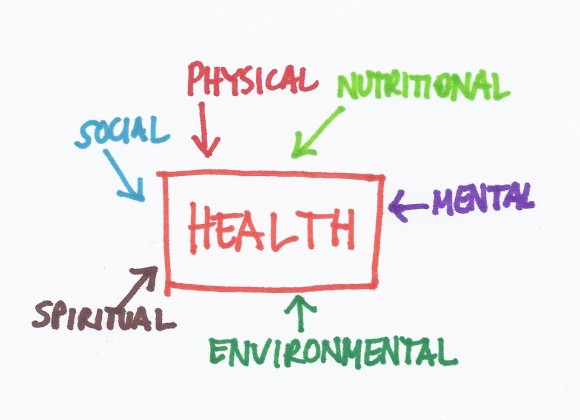 During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.
During my internship, I had an 18 year old patient with diabetes who I followed in my outpatient clinic (let’s call him Sam). He was first diagnosed at age 3 and had many hospitalizations thereafter for his poorly controlled diabetes. On one of these admissions, he arrived in the emergency room unconscious and near death because he hadn’t been taking his insulin. I happened to be on-call and stayed up with him all night managing his care. This required drawing blood tests every hour, adjusting medications, giving nutrients and fluids, etc. In the morning I had to present the situation to the physician in charge of my team at morning rounds. I proudly discussed how I had taken care of all of Sam’s problems throughout the night and how well he now looked. The senior physician asked me and the other interns and residents on our the team what the diagnosis was in this patient. We all looked at him like he was crazy since we had been talking about Sam’s diabetic emergency for the past 15 minutes. Then he told us that he thought the diagnosis was “communication failure”. Then we were convinced that he was crazy.
New types of evidence
It can be difficult to figure out how to use the results of research studies (randomized controlled trials or RCTs) to make a healthcare decision. There are many other problems with RCTs that may be less obvious.
First, to perform an RCT can take years – you need to get approval from the hospital where you are performing the study because you are doing research on humans. Then you need to get funding for the study so you may need to apply for some grants. After the study is completed, the results need to be analyzed; and then a paper needs to be written and submitted for publication to a journal. It could take years from the time the results are known until the time they are published.
Communication, Innovation and Organization
 The Care Triad doesn’t really work without three important foundations – communication, innovation and organization.
The Care Triad doesn’t really work without three important foundations – communication, innovation and organization.
Communication requires that all members of the healthcare team understand that the patient is the most important person on the team. Patients should be spoken to in a respectful way starting with the person who sits at the welcome desk. Doctors need to learn to translate complicated medical information into ways that patients can understand it and patients need to learn to ask questions when they don’t understand what the doctor is saying. Doctors (and other members of the healthcare team), patients and family members also need to learn to talk openly about the end of life. Patients may also find it helpful to communicate with each other in online communities. Both doctors and patients need to learn to use social media to help themselves and each other, recognizing the power of personal experiences.