Patient centered billing
 My husband and I returned from a weekend away to find a message on our answering machine saying that we owed money to the hospital and that if we didn’t pay it within 10 days, they would send the bill to a collection agency. The message was left on Saturday night and the automated voice said the charges were for cardiology services for our daughter.
My husband and I returned from a weekend away to find a message on our answering machine saying that we owed money to the hospital and that if we didn’t pay it within 10 days, they would send the bill to a collection agency. The message was left on Saturday night and the automated voice said the charges were for cardiology services for our daughter.
Our initial thought was that this was a mistake because: 1) our daughter had not been seen by a cardiologist and 2) we have paid all our bills.
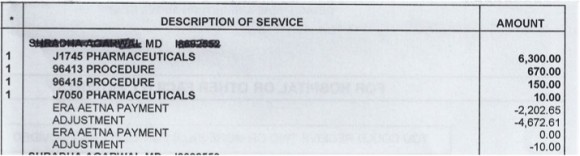
On Monday morning I called the billing office while making sure that I had plenty of work to keep me busy during the anticipated wait on hold (this turned out to be a good plan). Once someone came on the line (let’s call her the “customer service” representative) I explained the situation and gave her the account number that had been left on the answering machine. She told me I owed over $7000 and asked how I would like to pay it. I told her there must be some mistake because the bill was for my daughter who had not seen a cardiologist. She replied that “we say cardiology and other services” for all bills (does that make any sense to the patient?). Then I told her that I had paid a bill by phone on March 15 and gave her the confirmation number (thank God I took notes!) and the name of the person who took my payment (let’s call her Jane). Jane and I had had a lengthy conversation on March 15, going through the bill line by line so that I would understand it (despite working as a physician and a managed care medical director in the past and despite consulting with my physician husband I could not make any sense of it). The above excerpt from the bill includes one of 4 dates of service (note that I have blacked out the name of the treating physician but I didn’t recognize the name).
Here’s what Jane had explained to me on March 15:
- The hospital billed insurance $6,300 + $670 + $150 + $10 for a total of $7130.
- Our insurance allowed $2447.68 (I can’t figure out how to derive this amount from the billing statement but let’s accept it)
- Therefore we owe $244.74 because we pay 10% of charges once we meet our deductible (slight rounding error but close enough)
So, while I still couldn’t explain how the numbers were calculated, I could see that the amount of the final bill was consistent with the math for this particular date of service (I should mention that I was the kind of kid who did math problems for fun so I would really like to understand the math if I could). Getting back to the call on Monday, the “customer service” representative looked up my payment from March 15 and told me that I still owed money and asked me how I wanted to pay. There was now an edge to her voice and I asked her why she was not trying to help me. She gruffly told me to hold the line and in a few minutes, Jane (from the March 15 call) came on the line. Jane asked me why I had been rude to her colleague (really?). She told me in a frustrated tone that she would look into my bill and get back to me. When she called back, I was on another line (trying to get some work done) so she left a message which went something like this:
Please disregard the last message. Your bill is paid in full.
There was no apology and no acknowledgement that they had erroneously threatened me with a collection agency and treated me as a nuisance.
I have to say that the medical care my daughter received was focused on the patient but the billing department did not have the patient in mind at all:
- The primary focus was on collecting as much money as possible
- The naming of the billing department was based on their own internal language and made no sense to the patient (“cardiology and other services”)
- The physician of record was some behind-the-scenes person who we never met
- There was no attempt on the bill to explain where any of the numbers came from
- There was no acknowledgement during our conversations that the reason we had over $7000 in charges was that my daughter had been very sick (and perhaps this was a stressful time)
And that doesn’t begin to address the astronomical charges themselves! That’s for another day.
Dr. Nash…I agree payers have to do better. Very good example to show the problems in our industry. I am glad you shared the information as all consumers need to understand they do have a voice, a right and an obligation to ask questions about their care and the bills that go along with their care.
This week, I had a problem with my cell phone and I called ATT. The first person I talked to did not have a good rapport and I did not feel like we were ‘communicating’ well. She was an American (Not from a foreign country, but seemed ‘miffed’ that I had a problem. I asked her for someone else as I did not feel that we were working well together and she said that she was capable of helping me and refused to transfer me. I hung up, waited a few minutes and called back and got a second person who was welcoming and really helped me.
It should not be like this, but it is..customer service is important.
Regarding the bill/language of billing…..that is another issue..but healthcare companies need to instill into their teams the importance of patience, customer service and how to explain processes. This is something insurance companies are judged..via accreditation. People who get poor treatment by the hospital, by the insurance company or from their cell phone company need to fill in the survey’s that come out after the call so organizations have an idea about the services they are providing. I filled out the ATT survey and praised the person who was good and recommend the first person have additional training.
Thanks for your insights!