Month: December 2012
The Evidence
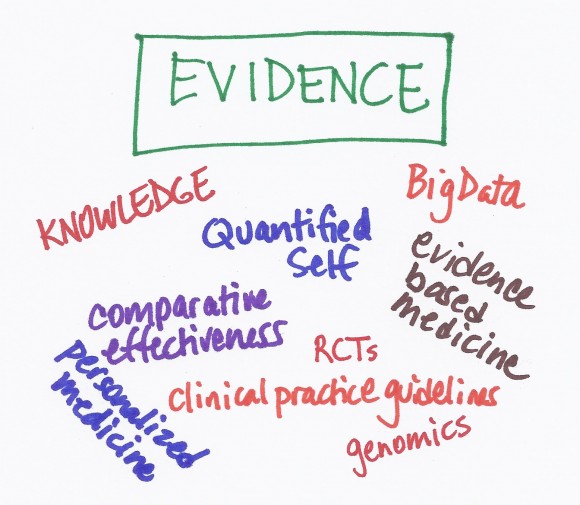 Before I went to medical school, I studied biology in college and did laboratory research. One of the reasons I went into medicine was that I liked science but like most doctors, I didn’t understand the science as well as I thought I did. The scientific literature – the studies that have been done to figure out which treatments work and which ones don’t – is what we call the evidence.
Before I went to medical school, I studied biology in college and did laboratory research. One of the reasons I went into medicine was that I liked science but like most doctors, I didn’t understand the science as well as I thought I did. The scientific literature – the studies that have been done to figure out which treatments work and which ones don’t – is what we call the evidence.
In many ways, the evidence is the most challenging part of the Care Triad.
During my medical training, I remember reading individual scientific papers and doing exactly what they said. That approach may be OK when there is only one study that has been done to look at a particular treatment. But once there are many studies available, you need to look at all of them and figure out what the totality of the research is saying. You might look at one study that says a particular treatment works but there may be 9 other studies that say the same treatment is useless. Focusing on one study is called “cherry picking” and lots of doctors do it without realizing it.
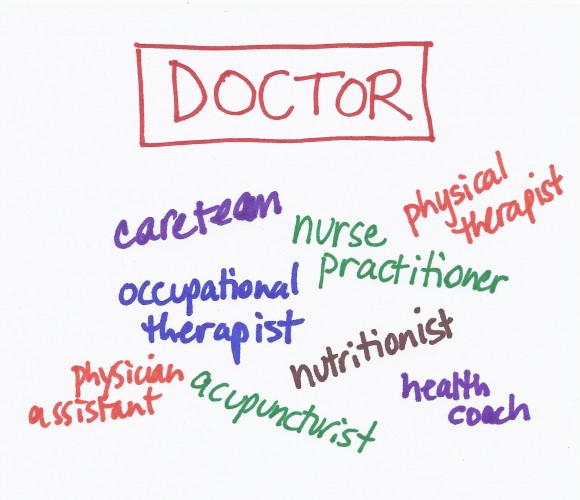
The Doctor
 I did my internal medicine residency at a city hospital where I knew I would have lots of autonomy and see a broad array of diseases. My coworkers and I were on-call every third night and were usually up all night. We did everything for ourselves – transporting patients from the emergency room to their hospital beds or to the x-ray department, drawing blood, etc. We were even expected to look at all of the patient’s laboratory specimens – urine, sputum, spinal fluid, etc. – under a microscope. We never asked a patient what he or she wanted – it never occurred to us that there was a choice.
I did my internal medicine residency at a city hospital where I knew I would have lots of autonomy and see a broad array of diseases. My coworkers and I were on-call every third night and were usually up all night. We did everything for ourselves – transporting patients from the emergency room to their hospital beds or to the x-ray department, drawing blood, etc. We were even expected to look at all of the patient’s laboratory specimens – urine, sputum, spinal fluid, etc. – under a microscope. We never asked a patient what he or she wanted – it never occurred to us that there was a choice.
Things are different now. It is impossible to keep up-to-date with all of the medical advances and there are now a huge number of tests available to diagnose diseases. No one person can manage all of the complexities of care so doctors have become more specialized. Medicine needs to become more of a team sport – where specialists work together as a team to help the patient. And doctors need to accept the roles of new types of care providers as team members such as physician assistants and nurse practitioners who may be especially suited to provide routine care. We also now recognize that physical therapy, occupational therapy and nutrition are integral elements of care and that stress management, acupuncture, weight loss, health coaching and numerous other interventions can improve health in certain situations. In addition to being able to work as part of a team and help coordinate the team, doctors need to recognize that the most important member of the team is the patient.
The Patient
 When I was a child, my parents were very friendly with their doctor who was an internist (someone who did medical training in internal medicine or general medicine for adults). Because he was a family friend, he agreed to start seeing me as a patient when I was about 12 years old. He was warm and friendly and took a long time to talk with me in his office before examining me. He did very few tests and almost never drew my blood.
When I was a child, my parents were very friendly with their doctor who was an internist (someone who did medical training in internal medicine or general medicine for adults). Because he was a family friend, he agreed to start seeing me as a patient when I was about 12 years old. He was warm and friendly and took a long time to talk with me in his office before examining me. He did very few tests and almost never drew my blood.
I remember those days fondly but they are long gone. My childhood doctor had far fewer tools at his fingertips and far less medical knowledge than we have today. Patients had very little access to the scant medical literature that was available. We put our trust in our doctors because they knew more than we did.
Welcome to Care Triad
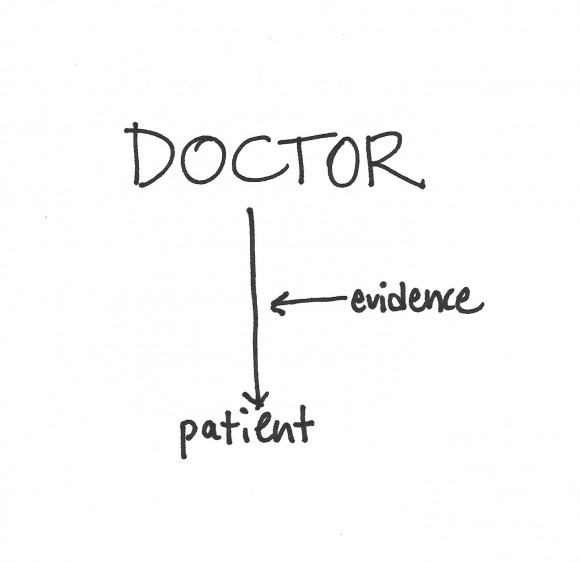
Healthcare is in the midst of a revolution. Our current healthcare system was designed for a simpler time when the doctor had all the power – understood the minimal evidence about what worked and what didn’t – and the patient was told what to do. Times have changed. The amount of new research published every day is staggering and no person could possibly keep up with it. Furthermore, the research has shown that there is often no single right answer to a medical problem – what is right for one patient may not be right for another. We’re also seeing remarkable advances in medical technology, social media, genomics and medical knowledge. Patients now have instant access to the original research and to other patients like them around the world. We need to rethink the way we design and administer healthcare to reflect the new alignment of the key elements of healthcare – the patient, the doctor and the evidence.
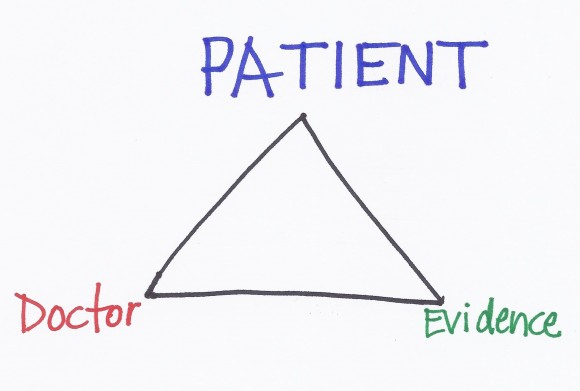
Optimal care today requires that the doctor, patient and evidence play more balanced roles – I call it the Care Triad. I put the patient at the top of the triangle because the patient is the most important person in making healthcare decisions. Because most healthcare decisions do not have a correct answer, the patient needs help from the doctor (using his or her experience) and the evidence (data about what really works) in order to make the best personal decision.
How do we pick our doctor? How do we know if the evidence is reliable? How do we make an informed decision? I’ll write about all these things. I’ll write about how the Care Triad is relevant when we are well and when we are ill, when we are at the beginning of life and the end of life. I’ll also write about the many factors that influence the Care Triad – communications, technology, social media, community, business processes and more.